If you suffer from Irritable Bowel Syndrome (IBS), you're well aware of the painful and sometimes embarrassing symptoms that come with it. Despite being a common condition, there's no cure for IBS, making it challenging to manage. However, there is an alternative approach that can help alleviate some of the symptoms - Intermittent Fasting (IF).
Understanding Intermittent Fasting and IBS
Intermittent Fasting, or IF, is a popular eating plan where one cycles between periods of eating and fasting. This approach doesn't restrict the types of food you can eat but focuses more on when you can eat. The idea behind IF is to give your digestive system a long break so that it can function better and more effectively.
What is Intermittent Fasting?
Intermittent fasting is a pattern of eating that alternates between periods of fasting, or not eating, and periods of eating. There are various methods of intermittent fasting, but the most common ones are the 16/8 method, the 5:2 method, and Alternate-Day fasting.
The 16/8 method involves fasting for 16 hours and eating within an 8-hour window. For example, you may choose to eat between 12 pm and 8 pm and fast for the remaining 16 hours of the day. The 5:2 method involves eating normally for five days of the week and restricting calories to 500-600 for the remaining two days. The Alternate-Day fasting method involves fasting every other day and eating normally on non-fasting days.
Intermittent fasting has been shown to have several health benefits, including weight loss, improved insulin sensitivity, reduced inflammation, and improved brain function.
What is Irritable Bowel Syndrome (IBS)?
IBS is a common gastrointestinal disorder that affects the large intestine. It can cause a wide array of symptoms, which include bloating, cramping, gas, constipation, diarrhea, and abdominal pain. These symptoms can be debilitating, leading to discomfort and frustration.
IBS is a chronic condition, and there is no cure for it. However, there are several ways to manage the symptoms and improve quality of life. These include dietary changes, stress management, and medication.
Common IBS Symptoms and Triggers
IBS symptoms are different for everyone, but some of the most common symptoms include abdominal pain, bloating, and changes in bowel movements. Triggers can include stress, certain foods, and hormonal changes. Keeping track of your symptoms can help you identify potential triggers.
Some studies have suggested that intermittent fasting may help alleviate some IBS symptoms. Fasting has been shown to reduce inflammation in the gut, which can help reduce symptoms like bloating and abdominal pain. However, more research is needed to fully understand the relationship between intermittent fasting and IBS.
In conclusion, intermittent fasting is a popular eating plan that can have several health benefits. If you have IBS, it's important to talk to your doctor before starting any new diet or lifestyle changes. While intermittent fasting may help alleviate some symptoms, it's not a cure for IBS, and individual results may vary.
The Science Behind Intermittent Fasting and IBS
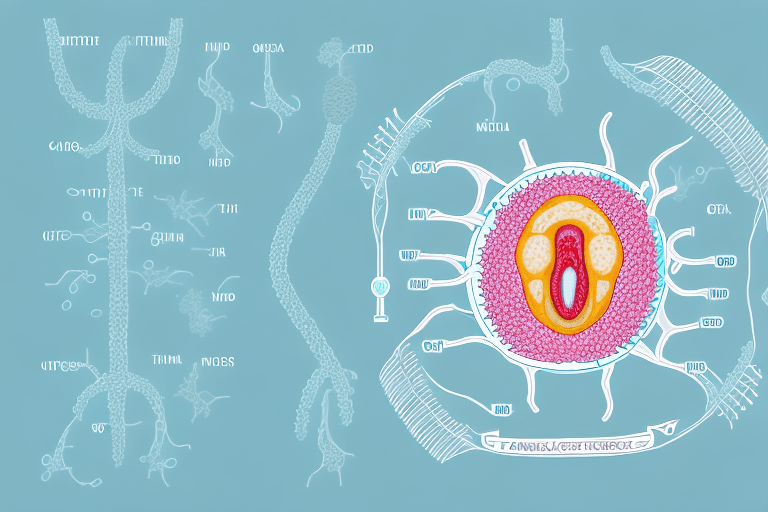
Recent studies have shown that intermittent fasting can have a significant impact on gut health. It can help reduce inflammation in the gut, which is one of the triggers for IBS symptoms. Fasting also helps to increase the number of beneficial bacteria in the gut, helping to improve overall gut health.
How Fasting Affects Gut Health
Fasting gives the digestive system a chance to rest and reset, which can help improve gut health. During the fasting period, the gut's inflammatory response is reduced, and the production of beneficial bacteria increases. This, in turn, can help reduce inflammation, which is a significant trigger for IBS symptoms.
Additionally, fasting can help improve the function of the gut's protective barrier. The gut barrier is a layer of cells that separates the contents of the gut from the rest of the body. When this barrier is compromised, harmful substances can leak into the bloodstream, leading to inflammation and other health issues. Fasting has been shown to help strengthen the gut barrier, reducing the risk of harmful substances entering the bloodstream.
Intermittent Fasting and Inflammation Reduction
Inflammation is a primary trigger for IBS symptoms. Recent studies have shown that intermittent fasting can help reduce inflammation in the digestive system, leading to a significant reduction in symptoms for those with IBS.
Intermittent fasting can also help reduce systemic inflammation throughout the body. Systemic inflammation is a type of inflammation that affects the entire body and has been linked to a range of health issues, including heart disease, diabetes, and cancer. By reducing systemic inflammation, intermittent fasting can help improve overall health and reduce the risk of chronic diseases.
The Role of Gut Microbiota in IBS and Fasting
Gut microbiota plays an essential role in gut health. They help keep harmful bacteria under control while aiding in digestion. Recent studies have shown that intermittent fasting can help change the composition of gut microbiota, leading to improved gut health and reduced symptoms for those with IBS.
Intermittent fasting can help increase the number of beneficial bacteria in the gut, while reducing the number of harmful bacteria. This can help improve the overall balance of gut microbiota, leading to improved gut health and reduced symptoms of IBS.
Overall, the science behind intermittent fasting and IBS is promising. By reducing inflammation, improving gut health, and balancing gut microbiota, intermittent fasting can help reduce the symptoms of IBS and improve overall health.
Different Intermittent Fasting Methods for IBS Management
Intermittent fasting has become a popular method for managing various health conditions, including Irritable Bowel Syndrome (IBS). It involves cycles of fasting and eating, with the aim of improving overall health and reducing symptoms of IBS. There are various methods of intermittent fasting, each with its own approach and benefits. Choosing the right one for you depends on your lifestyle, goals, and IBS symptoms.
The 16/8 Method
The 16/8 method is also known as the time-restricted feeding method. It involves skipping breakfast and restricting eating to an eight-hour period during the day, followed by a 16-hour fast. This means eating your last meal by 8 pm and not eating anything until noon the following day. This method is popular because it is easy to follow and fits well with most people's lifestyles. It also allows for flexibility in meal times, making it easier to plan meals around work, social events, and other activities.
In addition to its benefits for IBS management, the 16/8 method has been shown to improve insulin sensitivity, aid weight loss, and reduce inflammation in the body.
The 5:2 Method
The 5:2 method involves restricting calorie intake to 500-600 calories two days a week and eating a healthy diet for the remaining five days. This method is also known as the Fast Diet and has been shown to improve insulin sensitivity, aid weight loss, and reduce inflammation in the body.
For IBS management, the 5:2 method may be beneficial because it allows for some calorie restriction without the need for prolonged fasting. It also allows for flexibility in meal planning and can be adapted to fit individual dietary needs.
Alternate-Day Fasting
The alternate-day fasting method involves fasting for 24 hours, followed by a regular eating day, and repeating this cycle every other day. This method is more intense than the other two methods and may not be suitable for everyone. It requires strict adherence to the fasting and eating cycles and may cause hunger, fatigue, and other side effects.
However, alternate-day fasting has been shown to improve insulin sensitivity, aid weight loss, and reduce inflammation in the body. It may also be beneficial for IBS management because it allows for periods of rest and recovery for the digestive system.
Choosing the Right Method for You
Choosing the right method depends on your lifestyle and goals. It's important to consult with your doctor before starting any fasting method, especially if you suffer from IBS or any other health condition. Your doctor can help you determine which method is best for you and provide guidance on how to safely implement it.
In addition to intermittent fasting, other lifestyle changes may also be beneficial for managing IBS. These include stress reduction techniques, regular exercise, and a healthy diet rich in fiber and low in processed foods.
By incorporating these strategies into your daily routine, you can improve your overall health and reduce symptoms of IBS.
Tips for Successfully Implementing Intermittent Fasting with IBS
Gradually Introduce Fasting into Your Routine
Intermittent fasting has become increasingly popular in recent years for its potential health benefits, including improved digestion and weight loss. However, for individuals with IBS, it's essential to approach fasting with caution and gradually introduce it into your routine. Starting your fasting routine slowly is vital. This allows your body to adjust to the changes progressively. Begin by fasting for a shorter period and gradually increase the duration. It's also essential to listen to your body and adjust accordingly.
As you begin to fast, you may experience some initial discomfort, including hunger pangs, headaches, and fatigue. However, these symptoms should subside as your body adjusts to the new routine. If you experience persistent symptoms, it may be a sign that fasting is not suitable for you or that you need to adjust your fasting schedule.
Monitor Your Symptoms and Adjust Accordingly
Keeping track of your symptoms and how they relate to fasting can help you identify potential triggers and make necessary adjustments to your fasting routine. It's essential to pay attention to your body and note any changes in your symptoms during fasting periods. If you experience an increase in symptoms like bloating, gas, or abdominal pain, it may be a sign that you need to adjust your fasting schedule or seek medical advice.
It's also important to note that everyone's IBS symptoms are different, and what works for one person may not work for another. Therefore, it's essential to listen to your body and make adjustments accordingly.
Stay Hydrated and Maintain a Balanced Diet
Staying hydrated is crucial, especially during fasting periods. Drinking enough water and fluids can help with digestion and reduce the likelihood of constipation. It's recommended to drink at least eight glasses of water a day, but this may vary depending on your individual needs.
It's also important to maintain a balanced diet during eating periods. Including fruits, vegetables, and lean proteins in your meals can help improve digestion and reduce the risk of IBS symptoms. Avoiding trigger foods like high-fat foods, caffeine, and alcohol may also help reduce symptoms.
Consult with a Healthcare Professional
Before starting any fasting routine, talk to your healthcare provider, especially if you have an underlying health condition like IBS. They may help you determine if fasting is appropriate and safe for you and help create a customized plan to meet your health goals.
Your healthcare provider may also recommend working with a registered dietitian to ensure that your fasting routine is balanced and meets your nutritional needs. A registered dietitian can help you create a meal plan that includes healthy foods and ensures that you're getting all the nutrients your body needs.
In conclusion, implementing intermittent fasting with IBS requires a cautious and gradual approach. It's essential to listen to your body, monitor your symptoms, stay hydrated, maintain a balanced diet, and consult with a healthcare professional. With the right approach, intermittent fasting can be a useful tool in managing IBS symptoms and improving overall health.
Conclusion
Intermitting fasting can be an effective approach to manage IBS symptoms. By allowing the gut time to rest and resetting the digestive system, you can improve gut health and reduce inflammation. It's essential to choose the right fasting method for you and implement it gradually, keeping track of symptoms to adjust accordingly. As always, consult with a healthcare professional before starting any fasting routine.